Populaire dans votre secteur d’activité






























































Recherches associées:
















































































































































Meilleures catégories
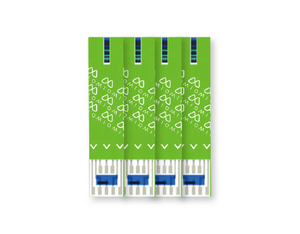
Concernant glucomètre lancette
Un équilibre glycémique sain est essentiel dans le traitement du diabète. Les glucomètre lancette fiables sur Alibaba.com sont livrés dans un kit complet prêt à l'emploi. Les compteurs sont faciles à utiliser avec des boutons de poignée visibles. De manière significative, les produits sont simples à maintenir en matière d'hygiène. De même, les calculs glucomètre lancette sont numériques avec une capacité à donner des données moyennes périodiques sur la glycémie. Avec des instructions simples, l'utilisateur peut nettoyer et stocker en toute confiance.
Le sang glucomètre lancette est rapide et donne des lectures précises sur place. Les données sont sûres et facilement récupérables en appuyant sur un bouton. Avec les glucomètres réutilisables, l'utilisateur aura moins de visites cliniques et économisera de l'argent. Les gadgets portables aident lors du transit d'une zone à une autre sans vérifier aucune clinique. Le stockage de données est volumineux, ce qui laisse de l'espace pour d'énormes collections d'entrée.
Lorsqu'il cherche à acheter le médical glucomètre lancette sur Alibaba.com, l'acheteur doit envisager l'utilisation principale. Le système technologique est crucial pour la distribution des données. Le coût de la maintenance et les conditions d'hygiène sont primordiaux. Les rappels aident dans les contrôles réguliers lorsque occupé. Il est donc préférable d’investir dans ce qui aide à développer une vie meilleure.
Les concurrents glucomètre lancette sur Alibaba.com sont attrayants et accueillants pour toutes les gammes d’acheteurs. Les fournisseurs fiables ont de meilleurs catalogues et des devis variés pour une expérience d'achat éclairée. Le public doit rechercher des connaissances pour une meilleure expérience d'achat et rajeunir un meilleur style de vie.